For clinicians
The Department will periodically contact patients waiting for an outpatient clinic appointment via SMS, with a link to an electronic form. This is part of routine waitlist auditing to ensure patient details are up to date. If you receive this SMS, please update your details.
Refer to Specialist Outpatient Service
Patients can be referred to specialist Outpatient Services from:
- General practitioners (GPs)
- Medical practitioners within the hospital (e.g. Emergency Department, inpatient units)
- Medical practitioners' private rooms
- Medical practitioners in other hospitals (transfer)
- Other health care professionals (e.g. optometrist to ophthalmologist).
The clinical assessment criteria and the administrative requirements for referring a patient to specialist Outpatient Services are the same irrespective of the source of referral. This includes all referrals made by medical and other practitioners from within the hospital to Outpatient Clinics.
An approved specialist referral form (template), either electronic or paper, should be submitted by the referring practitioner for all patients regardless of the source of the referral; however well-written and complete referral letters will be accepted as long as all the required information is included.
Referral Standards
Referrals to specialist Outpatient Services must be submitted electronically as an eReferral (preferred method) or in writing (e.g. letter, facsimile, electronic file) and should include the following information:
- The patient's full name (or alias) and where appropriate (e.g. for a minor) the name of the parent or caregiver
- The patient's address
- The patient's telephone number (home and alternative)
- The patient's date of birth
- Next of kin/carer/guardian/local contact for paediatric referrals
- Hospital Unit Medical Record Number (UMRN) and Medicare number (if known)
- Past history including details of previous treatment, investigations including x-rays (photocopied results and films where appropriate)
- Presenting symptoms and their duration and details of any associated medical conditions which may affect the presenting condition, or its treatment (e.g. diabetes)
- Details of current medications and any drug allergies, GP diagnosis and categorisation with reference to the pre-referral guidelines where available
- Details of current and relevant past medications
- Allergies and drug intolerances
- Date of referral, details of referring practitioner and GP details if different from the referring practitioner and the name of the doctor/ clinic to which the patient is being referred
Patients being re-referred with the same problem will have a letter containing the relevant information directed to the original specialist who will arrange an appropriate follow-up appointment at a routine clinic.
The use of the standard referral template, either electronic or paper-based, is recommended to ensure the provision of adequate referral content.
THS will ensure referrals include adequate information to allow categorisation, prioritisation and direction of patients to appropriate services as per the pre-referral guidelines for First Specialist Assessment.
THS will implement procedures to inform referring practitioners with respect to appropriate referral content, such as the THS Outpatient Website.
Referring practitioners will be encouraged to meet referral requirement through regular feedback processes (e.g. via the eReferrals solution, telephone, letter).
THS will identify inadequate or incomplete referrals and, where necessary, return the referral for more complete information.
eReferrals
The Tasmanian Department of Health has partnered with Primary Health Tasmania to introduce an eReferral solution to Tasmania’s health system.
eReferrals are an important way to improve the quality and timeliness of referrals across primary care and into public hospital outpatient services, ensuring the right information follows the patient between care settings and providers.
The eReferral solution was rolled out progressively to Tasmanian outpatient facilities at the Launceston General, North-West Regional, Mersey Community and Royal Hobart Hospitals, and is currently being expanded to include additional community and outpatient services.
Where available, eReferrals are the preferred method for referral to Outpatient Clinics across the THS.
See the Quick Guide to creating an eReferral or visit the Tasmanian eReferral System for more information.
Pre-referral Guidelines
To ensure patients are receiving the most appropriate care within the desired timeframe, referring healthcare providers should ensure that the referral includes all history, examination and examination findings listed in the pre-referral guidelines.
Referral Non-acceptance
Referrals to Outpatient clinics undergo a triage process prior to an appointment being made. Referrals that do not have all the requested information and investigations for triage will not be accepted and will be returned for a number of reasons.
- The referral is missing details of Medical Imaging marked as required in the Outpatient guidelines. The Medical Imaging requested is essential to allow efficient triage to be made and is usually more quickly obtained in general practice.
- The referral is missing details of Pathology investigations marked as required in the Outpatient guidelines. The Pathology investigations requested are essential to allow efficient triage to be made and are more quickly obtained in general practice.
- The referral does not contain the required clinical, past and/or family history requested to ensure efficient triage. The list was developed from national best practice guidelines.
- Some THS services are not provided on an outpatient basis.
- Referrals must be legible to ensure that no mistakes are made in the triage process and therefore referrals that cannot be read easily, and may lead to confusion, will be returned.
- In order for an appointment to be made it must be possible to identify and contact the patient, this includes details of parents/guardian in the case of a minor. All referrals with insufficient demographic information will be returned to the referrer.
- The requested service is Not Routinely Funded.
- The THS has developed guidelines to ensure that patients are seen by the most appropriate clinician and these guidelines are publically available. It is requested that referrals are made to the correct service.
- When the patient’s condition has significantly changed a new or updated referral needs to be sent. A patient’s position on the waiting list will not be reviewed by the resending of the original referral without additional information.
- A number of services are not offered at the THS as they are better managed in the community. These services are listed on the relevant pages.
Where there is dispute about the non-acceptance of a referral a letter should be sent to the clinic in the first instance. It will then be appropriately investigated including referral to General Practice Liaison.
Active Life of Referral
As per the Medicare referral rules outlined in A Guide to Medicare and other HIC health programs available at www.medicareaustralia.gov.au, referrals issued by:
- A GP to a specialist referral remains valid for a single course of treatment (an episode of care) or for a period of 12 months from the initial specialist outpatient consultation, whichever is the lesser. GPs can indicate a shorter, longer or indefinite period for referral.
- A specialist to specialist referral remains valid for a single course of treatment (an episode of care) or for a period of three months from the initial specialist outpatient consultation, whichever is the lesser.
An episode of care commences at the initial consultation, continues through treatment and concludes when the patient is returned to the care of the referring practitioner.
On the occasion of referral for chronic or long-term conditions that will extend beyond three or 12 months, the referring practitioner will detail the patient's clinical condition and whether they will require continuing care and management by a specialist. Examples of these may include Renal and Oncology referrals. In these instances, wording on the referral must indicate that the referral is valid for an indefinite period.
Unrelated Condition
The presentation of an unrelated illness or condition which may result in another course of treatment (episode of care) in another specialty will require a new referral for first specialist assessment. In such cases the treating specialist will refer the patient to their GP for management.
In extraordinary circumstances a treating specialist may elect, on clinical urgency grounds, to directly on-refer to another specialty within the hospital. In such cases the pre-referral guidelines (where available) will be applied by the referring specialist.
Timeliness of First Specialist Assessment
If at the time a referral is received, or at any time thereafter, the hospital considers that a specialist is unable or is unlikely to be able to provide assessment or treatment within the recommended timeframe, the hospital will take responsibility for expediting access to care. Options available in the first instance include:
- Transferring the referral (which may require seeking a new referral from the GP) to another specialist within the same hospital
- Transfer the referral (which may require seeking a new referral from the GP) to another hospital where an earlier outpatient appointment can be provided
- Having the patient reviewed by nursing or allied health staff
Clinical Monitoring of Patients on the Outpatient Services Wait List
- The referring practitioner will assume the responsibility for clinical monitoring and communication to facilitate timely and appropriate clinical management of their patients registered on the Outpatient Service wait lists who are awaiting initial consultation
- Referring practitioners will be notified of the need to monitor the patient's clinical condition and communicate any changes to their condition
- Referring practitioners will be asked to notify the facility in writing of any changes to the patient's clinical status - the need for subsequent re-categorisation will then be considered by the triaging clinician
Communication
Appropriate and timely communication is vitally important when providing information about Outpatient Services to patients, referring practitioners and health care professionals. If available, the preference is utilising the eReferrals platform as this facilitates timely communication between Outpatient Services and the referrer.
Categorisation of Referral
For more information about how referrals are categorised for priority, please see Categorisation of Referral
Wait List System
Facilities will maintain a wait list to register essential details about all patients requiring Outpatient Service consultation.
Removal from the Outpatient Service Wait List or Appointment Schedule
Reasons for removal from the Outpatient Service wait list or appointment schedule include:
- Patient request to have name removed
- Clinical review or administrative audit ascertains that Outpatient Service attendance is no longer required
- Advice that the patient has been or will be attending elsewhere for treatment of the same condition
- The patient:
- Has declined the offer of a clinic appointment without valid reason
- Has not presented for a booked clinic appointment and has not contacted the facility
- Has not responded to audit measures and cannot be located
- Is deceased
- View the indicative outpatient appointment waiting times
Interpreter Service
The THS Interpreter Booking Service (IBS) provides professional interpreters, free of charge to assist non-English speaking and hard of hearing patients.
On-site interpreters are supplied for all outpatient appointments and hospital stays for patients who need one. Where no on-site interpreter can attend, a telephone or remote video interpreter will be used instead. For full information on this service please see THS - Interpreter Services | Tasmanian Health Service.
Procedures Not Routinely Performed
Principles: Patients should be referred by surgeons to Tasmanian public hospital waiting lists only when surgery meets an identified clinical need to improve the health of patients. Prioritisation of surgery will occur according to clinical need. These principles apply to both public and privately insured patients.
Tasmania has a set of defined procedures that are not funded to be routinely performed. However, some procedures can occur in exceptional circumstances where patients:
- meet one or more of the exceptional clinical indications for surgery
- have “other” circumstances which demonstrate an overriding need for surgery. These circumstances will be at the discretion of the Director of Surgery / Nursing Director of Surgery of the public hospital to which the patient was referred.
Refer to the approval process and guidelines for appeals.
Procedures Not Routinely Performed
Specialty: Plastic Surgery | |
Body Contouring Procedures | Skin and Subcutaneous Tissue Procedures |
Abdominal lipectomy | Hair transplant |
Abdominoplasty | Tattoo removal procedures |
Apronectomy | Removal of skin lesions (e.g. skin tags) |
Liposuction | Revision of scar |
Other skin excisions for contour e.g. buttock, thigh and arm lift |
|
Breast Procedures | Urological and Gynaecological Procedures |
Breast reduction (unilateral and bilateral) | Lengthening of penis procedure |
Breast augmentation (unilateral and bilateral) | Insertion of artificial erection devices |
Mastoplexy (breast lift) | Reversal of sterilisation |
Removal of breast prosthesis /Revision of breast augmentation | Gender reassignment surgery |
Nipple eversion (for nipple inversions) | Genital surgery aimed at improving appearance |
Nipple and/or areola reconstruction | Testicular prostheses |
Facial Procedures | Vascular Procedures |
Facelift | Varicose Vein procedures |
Reduction of upper or lower eyelid |
|
Aesthetic Rhinoplasty/Rhinoseptoplasty |
|
Correction of bat ear(s) (>19 years old) |
|
Repair of external ear lobes |
|
Guidance For Clinicians - Exceptional Clinical Indications For Surgery
Specialty: Plastic Surgery | |
Body Contouring Procedures | |
Procedure | Exceptional clinical indications for surgery |
Abdominal lipectomy Abdominoplasty Apronectomy | Correction of scarring as a result of previous abdominal surgery or trauma Disabling or persistent physical discomfort Intertrigo Post morbid obesity treatment where clinical symptoms present (erg intractable intertrigo) and BMI is <28 Required for hernia repair or other abdominal surgery Poorly fitting stoma bags |
Liposuction | Post traumatic pseudolipoma Lipodystrophy with BMI Gynaecomastia with BMI Lymphoedema Flap reduction Above conditional on BMI <28 |
Other skin excisions for contour, e.g. buttock, arm, thigh lift | Post-morbid obesity treatment where clinical symptoms present (e.g. intractable intertrigo and BMI is <28 |
Breast Procedures | |
Procedure | Exceptional clinical indications for surgery |
Breast reduction (bilateral/unilateral) | Female: Post mastectomy surgery where BMI < 28 Chronic head, neck and back ache (where pain is due to breast size) and/or chronic intertrigo. Male (gynaecomastia): Suspected malignancy Pain, 19 years or older, must have been present for more than 2 years and BMI < 28 Following treatment for cancer of the prostate This procedure is not provided to patients with a BMI > 35. |
Breast augmentation (bilateral/unilateral) | Malformation due to disease, trauma or a congenital condition (but not as the result of previous cosmetic surgery as a privately insured patient). |
Mastopexy (breast lift) | Post morbid obesity treatment where clinical symptoms present (e.g. intractable intertrigo) and BMI is <28 |
Removal of breast prosthesis/ Revision of breast augmentation | Removal of breast prosthesis and revision of breast augmentation - rupture, Infection or capsular contracture Revision of breast augmentation – as a part of treatment for breast cancer and reconstruction. |
Nipple eversion (for nipple inversions) | None |
Nipple and/or areola reconstruction | When performed as a part of a breast reconstruction due to disease or trauma (but not as the result of previous cosmetic surgery). |
Facial Procedures | |
Procedure | Exceptional clinical indications for surgery |
Facelift | Congenital facial abnormalities Facial palsy Specific conditions affecting the facial skin e.g. cutis laxa, pseudoxanthomaelasticum, neurofribromatosis To correct the consequences of trauma To correct deformity following surgery (where the primary procedure was not cosmetic) |
Reduction of upper or lower eyelid | Visual impairment |
Aesthetic Rhinoplasty/Rhinoseptoplasty | |
Correction of bat ear(s) >19 years | None |
Repair of external ear lobes | Post-traumatic surgery i.e. repair of acute laceration, but not as the result of use of expander devices. |
Skin and Subcutaneous Tissue Procedures | |
Procedure | Exceptional clinical indications for surgery |
Hair transplant | Treatment of alopecia due to disease or trauma. |
Tattoo removal procedures | None |
Removal of skin lesions (e.g. skin tags) | Suspected malignancy Obstruction of orifice or vision Facial disfigurement Recurrent infection Function limitation on movement or activity Pain Located on a site where they are subjected to trauma. |
Revision of scar | Where scar is the result of surgery, disease or trauma Where scar is the result of neoplastic surgery and is disfiguring and extensive. |
Specialty: Urology and Gynaecology | |
Procedure | Exceptional clinical indications for surgery |
Lengthening of penis procedure | Congenital abnormalities in children. Recurrent urinary tract infections where the patient is at risk of requiring renal dialysis. |
Insertion of artificial erection devices | Patients using urodomes Spinal patients with neurological erectile dysfunction. |
Reversal of sterilisation | None |
Gender reassignment surgery | Congenital abnormalities in children. |
Genital surgery aimed at improving appearance Circumcision | Patients requiring prostheses following orchidectomy Phimosis, Urinary Tract Infection, Carcinoma of penis |
Testicular prostheses | Following orchidectomy for malignant disease. |
Specialty: Vascular Surgery | |
Procedure | Exceptional clinical indications for surgery |
Varicose vein procedures | Chronic leg swelling, chronic dermatitis, leg ulcers or foot infections that fail to heal as a result of severe varicosities causing chronic stasis and venous ulceration. Objective clinical evidence of chronic venous insufficiency. Recurrent (more than 2 episodes superficial thrombophlebitis). |
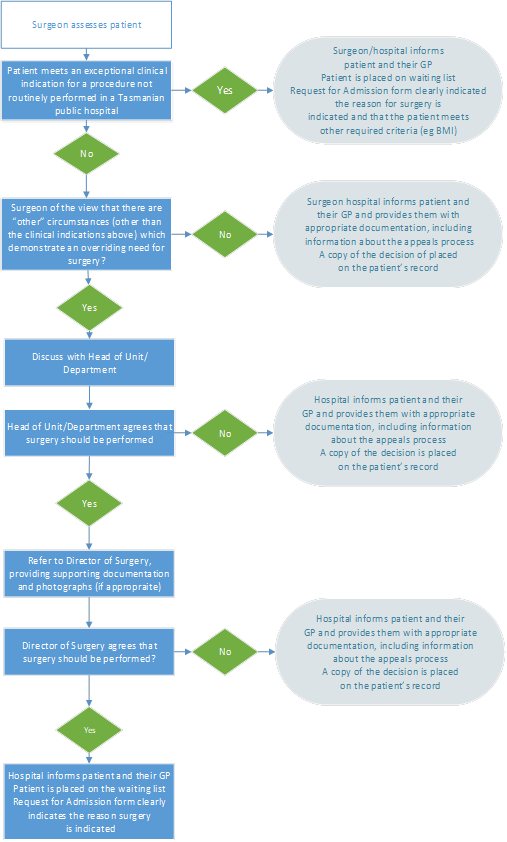
Approval Process and Guidelines for Appeals
Hospital Approval Process
If a surgeon assesses a patient as meeting the exceptional clinical indications for surgery, the Request for Admission (RFA) form should be completed and the patient placed on the elective surgery waiting list in accordance with hospital processes.
If a surgeon is of the view that a patient has “other” circumstances (other than the exceptional clinical indications listed) which demonstrate an overriding need for surgery, the Director of Surgery or, in certain circumstances, the Statewide Surgical and Perioperative Services Committee must give their approval for surgery to proceed.
The Hospital Approval Process Flow Chart details the process to be followed should a surgeon be of the view that a patient requires a procedure not routinely performed in Tasmanian public hospitals.
- If, after assessing the patient, the surgeon deems the patient meets an exceptional clinical indication for a procedure not routinely performed in a Tasmanian public hospital, the surgeon/hospital informs the patient and their GP. The patient is placed on the waiting list. The Request for Admission must clearly indicate the reason surgery is indicated and that the patient meets other required criteria (e.g. BMI).
- If there are no “other” circumstances (other than the clinical indications above) which demonstrate an overriding need for surgery, the surgeon/hospital informs the patient and their GP and provides them with appropriate documentation, including information about the appeals process. A copy of the decision is placed on the patient’s record.
- If the patient does not meet an exceptional clinical indication, but the surgeon is of the view that there are “other” circumstances (other than the clinical indications above) which demonstrate an overriding need for surgery, then the surgeon discusses this with the Head of Unit/Department.
- If the Head of Unit/Department does not agree that surgery should be performed, the hospital informs the patient and their GP and provides them with appropriate documentation, including information about the appeals process. A copy of the decision is placed on the patient’s record.
- If the Head of Unit/Department agrees that surgery should be performed, the case is referred to the Director of Surgery, with supporting documentation and photographs (if appropriate).
- If the Director of Surgery agrees that surgery should be performed, the hospital informs the patient and their GP. The patient is placed on the waiting list. The Request for Admission form must clearly indicate the reason surgery is indicated.
- If the Director of Surgery does not agree that surgery should be performed, the hospital informs the patient and their GP and provides them with appropriate documentation, including information about the appeals process. A copy of the decision is placed on the patient’s record.
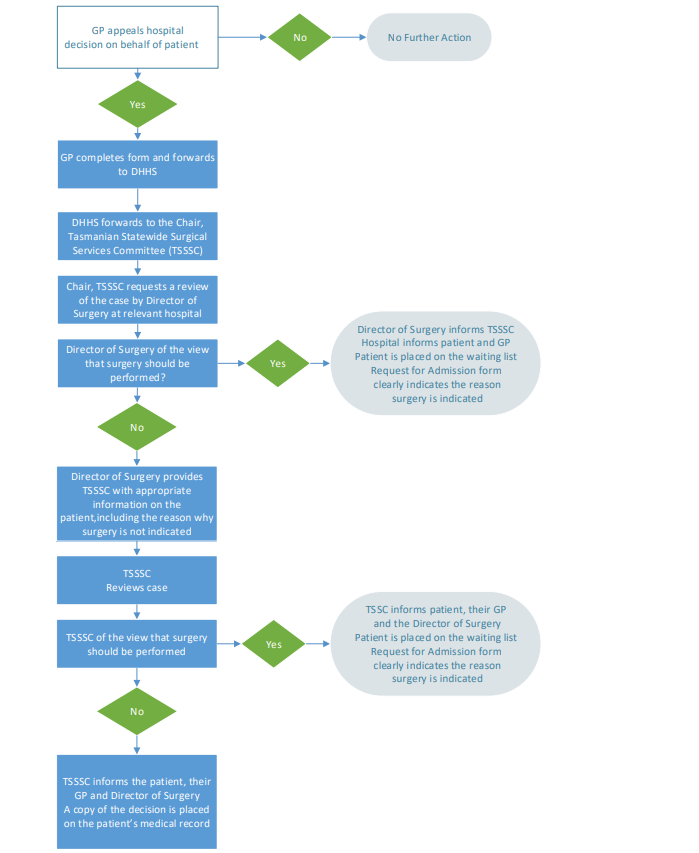
Patient Appeals Process
If a patient is referred to a public hospital for a procedure listed in these guidelines and surgery is declined, an appeal can be requested by the patient via their General Practitioner (GP). As patients usually cannot undergo a procedure without the referral of a GP, patients are not permitted to appeal on their own behalf.
Occasionally patients are referred to a private surgeon from a hospital emergency department. In this instance, the patient’s GP continues to be the most appropriate person to appeal on their behalf. Appeals must be made in writing to the Tasmanian Statewide Surgical and Perioperative Services Committee (TSSSC) by completing the form available at http://doh.health.tas.gov.au/hospital/elective_surgery which can also be provided from the surgical services department regionally.
The TSSSC will make its determination in consultation with the Director of Surgery of the hospital where the patient was assessed. The decision of the TSSSC will be communicated in writing to the Director of Surgery and to the patient’s GP. A copy of this decision is to be placed on the patient’s medical record at the hospital. See Patient Appeals Process Flowchart.The patient appeals process is as follows:
- If the patient’s GP agrees to appeal the hospital decision on behalf of the patient, the GP completes the GP Appeals Form and forwards it to the Department of Health. If the GP does not appeal on behalf of the patient, no further action can be taken.
- The Department of Health forwards the GP Appeals Form to the Chair, TSSSC. The Chair requests a review of the case by the Director of Surgery at the relevant hospital.
- If the Director of Surgery is of the view that surgery should be performed, the Director of Surgery informs the TSSSC, and the hospital informs the patient and GP. The patient is placed on the waiting list. The Request for Admission form must clearly indicate the reason surgery is indicated.
- If the Director of Surgery is of the view that surgery should not be performed, the Director of Surgery provides the TSSSC with appropriate information on the patient, including the reason why surgery is not indicated. The TSSSC reviews the case.
- If the TSSSC is of the view that surgery should be performed, the TSSSC informs the patient, their GP and the Director of Surgery. The patient is placed on the waiting list. The Request for Admission form must clearly indicate the reason surgery is indicated.
- If the TSSSC is of the view that surgery should not be performed, the TSSSC informs the patient, their GP and the Director of Surgery. A copy of the decision is placed on the patient’s medical record.
Hospital Approval Process Flowchart
Patient Appeals Process Flowchart
Source: Wait List Access Policy Handbook Review Date: June 2023
Feedback
If you have feedback or suggestions to improve this website, please let us know by emailing onlineservices@dhhs.tas.gov.au